Acute Fatty Liver of Pregnancy is Rare, But it Brings Attention to Racial Disparities Within Black Maternal Healthcare

By Joy Stephenson-Laws, JD, Founder
“It’s part of pregnancy,” is what 34-year-old expecting mother Jasmine Patton, who complained of uncomfortable symptoms, was told during one of her weekly doctor visits, according to a report from Good Morning America.
Very sadly, it was so much more than typical pregnancy discomfort, and Patton died of a condition called acute fatty liver of pregnancy (AFLP). She is survived by her husband and baby girl.
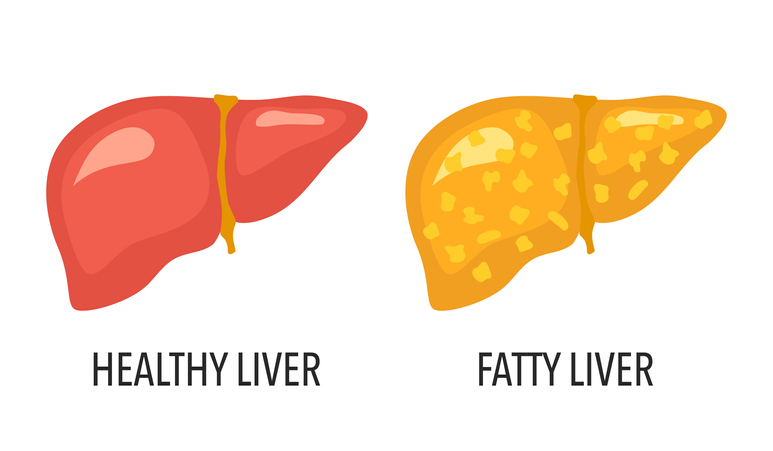
Fatty liver is an issue I have previously discussed a lot, however, not in regards to pregnancy.In general, fatty liver disease is an accumulation of excess fat in the liver. An excessively fat liver is an unhealthy and possibly damaged liver.
There is alcoholic fatty liver disease, also called alcoholic steatohepatitis, which a person can develop from drinking alcohol excessively. Then there is non-alcoholic fatty liver disease (NAFLD), which can occur in people who drink little to no alcohol. A fatty liver may be caused by being overweight or obese. People who carry a lot of belly fat (visceral fat) are especially prone to developing NAFLD.
First, I think it is important to acknowledge that AFLP is rare.
“Extremely rare. Never heard of any colleagues having such during my time in practice,” said Leonard Lawson, a recently retired obstetrician who practiced for more than 40 years and has delivered more than 4,000 babies, during an interview with pH Labs.
According to a report published by the National Institutes of Health (NIH), AFLP occurs in about five cases per 10,0000 pregnancies.
Just like alcoholic fatty liver disease and NAFLD, AFLP entails having liver cells that have an excessive amount of fat which can be damaging to the liver. Where AFLP differs, “Healthcare providers don’t know the exact cause of AFLP,” according to Stanford Medicine.
So it does not appear to be caused by diet or being overweight. In fact, Stanford reports that AFLP is more likely to happen in a thin person.
“Fats called triglycerides and fatty acids are normally broken down in the liver. But with AFLP your body makes too much of these. Research shows that AFLP may be an inherited problem with how the liver breaks down fats,” according to Stanford.
AFLP happens in the third trimester of pregnancy or during the earlier part of the postpartum period.
“Acute fatty liver in pregnancy (AFLP) is an obstetric emergency and carries high morbidity and mortality, including death in the mother and her fetus. It is characterized by maternal liver failure. Maternal mortality has decreased to 4% in recent years due to quicker diagnosis and immediate delivery,” according to this report published by the National Institutes of Health (NIH).
AFLP can be difficult to diagnose.“Early diagnosis of AFLP sometimes can be difficult because it shares features with other common conditions such as pre-eclampsia, viral hepatitis and cholestasis of pregnancy. However, a careful history and physical examination, in conjunction with compatible laboratory and imaging results, are often sufficient to make the diagnosis, and liver biopsy is rarely indicated,” (NIH).
There is a lot more to the tragic story of Jasmine Patton.
As an African-American woman particularly, Jasmine was very concerned about having a baby, her husband Edgar Patton discussed, in the report from Good Morning America.
“Black women in the United States (U.S.) disproportionately experience adverse pregnancy outcomes, including maternal mortality, compared to women of other racial and ethnic groups. Historical legacies of institutionalized racism and bias in medicine compound this problem,” according to another recent report published by the National Institutes of Health (NIH).
“Black women have a maternal mortality rate of 2.9 times that of White women in the United States.”

In the report from Good Morning America, Jasmine’s husband Edgar said that she had a very difficult pregnancy. She experienced extreme morning sickness in the first two trimesters as well as shortness of breath and extreme fatigue throughout her entire pregnancy. When she got close to her due date, Edgar expressed that things got really bad. Jasmine was so fatigued that she stayed in bed and could not eat. Her mood changed, and she couldn’t even go to work.
During this time, Jasmine, who was 34-years-old, was visiting her doctor weekly. As mentioned earlier, she was told that these extreme symptoms were just a “part of pregnancy.”
In a very sad turn of events, Jasmine’s health got so bad that she had to be taken to the hospital one day via ambulance. Her daughter was born via emergency cesarean section. Two days later Jasmine died of liver failure due to acute fatty liver of pregnancy.
“My concerns are as follows…,” said Leonard Lawson, the former obstetrician referenced earlier.
“1. Did the physician ignore the patient’s complaints? 2. Over what period of time did her condition deteriorate? 3. Were lab tests done? (her liver function tests would have been abnormal). 4. Would consultation with other physicians (internal or external perinatal medicine have led to an earlier diagnosis and intervention and a better outcome?”
I believe these are very valid concerns. It does not sit well with me that Jasmine was told that it was just a “part of pregnancy.” Stories of black women dying of pregnancy complications are way too common.
- Dr. Chaniece Wallace, a black pediatrician, died two days after giving birth to her daughter. She had symptoms of preeclampsia, and it appears that a late diagnosis, which could have been avoided, ultimately caused a lot of complications and her death. Black women also have higher rates of preeclampsia compared to white women.
- Shalon Irving died three weeks after giving birth due to complications from high blood pressure.
- Kira Johnson died from massive internal bleeding after having a planned cesarean section.
(pH must-read - How To Be Proactive About Preeclampsia and Your Baby’s Health With Vitamin D)
Sadly, a simple Google search of young black mothers dying from childbirth produces multiple news stories. You might have heard of the story of Tori Bowie, an Olympic track star who also died of complications due to childbirth.
"You know your body better than anybody,"Jasmine’s husband Edgar said.
"If you feel something is not right, regardless of what they tell you is normal or is common, if you feel it's not right, it's always OK to get a second opinion. That's the biggest thing."
(pH must-read - Untreated Anemia Can Be Deadly)
Even Serena Williams, who is obviously very famous and wealthy and can afford the best of care, had to speak up and demand attention for her concerns. When she gave birth for the first time via emergency cesarean section, she feared that she had a blood clot.
“The nurse suggested that Williams’ pain medication must be making her confused,” according to a report from Harvard Public Health.
Williams spoke up and explicitly stated what she needed to be tested for. As a result, several blood clots were discovered. Patients should not have to convince medical staff of the care they need, but the reality is that oftentimes it is necessary to speak up and perhaps even seek multiple opinions.
I highly recommend checking out this previous pH blog - Be Proactive About Racial Bias in Healthcare. And, as always, it is imperative for us all to take ownership of our health by eating healthily, being physically active, getting a sufficient amount of good quality sleep and getting routine nutrient tests.
For more blogs on pregnancy, click here.
Enjoy your healthy life!
Disclaimer: This article is not intended to provide medical advice. Please consult with your doctor or another competent healthcare practitioner to get specific medical advice for your situation.
The pH professional health care team includes recognized experts from a variety of health care and related disciplines, including physicians, attorneys, nutritionists, nurses, and certified fitness instructors. This team also includes the members of the pH Medical Advisory Board, which constantly monitors all pH programs, products, and services. To learn more about the pH Medical Advisory Board, click here.







