Another Reason to Consider the Emsella Chair for Incontinence – Your Future Health

By Joy Stephenson-Laws, JD, Founder
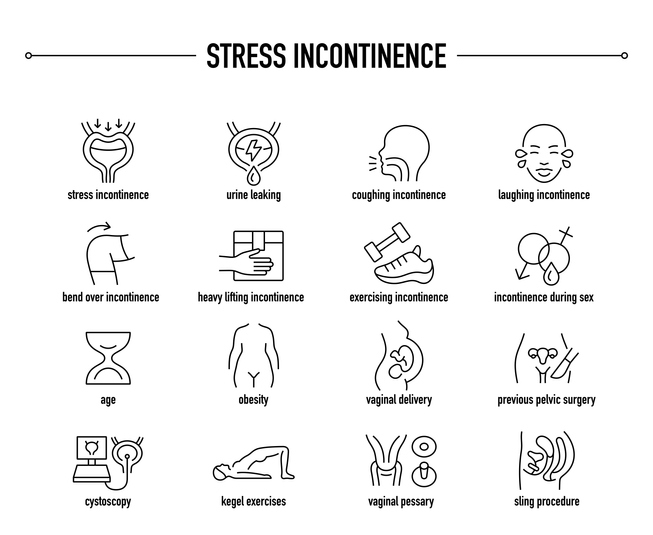
I recently blogged about the benefits of the Emsella Chair and how it may be your answer to managing urinary incontinence. To recap a bit, urinary incontinence - a loss of bladder control that can cause everything from small leaks to not being able to make it to the bathroom - typically becomes more common as we age. Almost 60 percent of older women experience it at some point. It usually happens when a person coughs, laughs, sneezes, or exerts themselves physically. This type of common incontinence is known as stress incontinence. Not being able to make it to the bathroom is known as urge continence. Clearly, any degree of incontinence can have a negative impact on your quality of life.

The Emsella Chair is a non-invasive, FDA-approved treatment for urinary incontinence. It works by delivering electromagnetic energy that triggers over 11,000 pelvic floor muscle contractions over the course of a 30-minute treatment. This is far more than you would be able to achieve doing kegel exercises on your own. There is no recovery time, so you can return to your daily routine immediately after a treatment session.
If helping manage current urinary incontinence were not enough reason to try the Emsella Chair, recent credible research may give women another reason to consider this treatment.
A study published in the medical journal Menopause, for example, suggests that urinary incontinence may increase your risk for other health issues and disabilities in the future. Researchers found that mixed incontinence had the highest correlation with disability issues, along with daily incontinence and larger amounts of incontinence.
One of the study’s authors commented that since the research suggests that urinary incontinence is associated with disability, “exploring treatment options in the early stages may help decrease this outcome in midlife women." One such treatment option could be the Emsella Chair (available at pH Lab’s health center in Encinitas).
Urinary incontinence is a predictor of high mortality.
Other studies about the link between urinary incontinence and future disability support the study published in Menopause. One reported that there seems to be a strong association with urinary incontinence and disabilities such as issues with mobility and interacting with others after fewer than four years. Another, an even more concerning one, suggests that urinary incontinence is a predictor of higher mortality in both the general and older populations. It also found, like the study published in Menopause, that the association increases with the severity of the incontinence. Researchers did point out that they are not sure if this association between incontinence and mortality is causative or just reflects a general impaired health condition.
One other found that women with urinary incontinence have a higher risk of declining mobility one year after suffering a hip fracture. Last, but not least, is another study which found that urinary incontinence may play a role in whether a person believes they should consider moving into a nursing home or other long-term care institutions.
Nutrition is always relevant too.
Whether you decide to use the Emsella Chair or other treatments to manage your incontinence, it’s important to not overlook the role nutrition can play in addressing different forms of incontinence and in complementing whatever your treatment regimen is. After all, good nutrition and diet are the cornerstones of a healthier life so it just follows that they can also play a role in managing urinary incontinence.
In order to be proactive about incontinence, you may want to check your nutritional status. This usually ensures your body is getting the nutrients it needs – and in the right amounts – to put you in the best position to manage your weight and help your body defend against disease such as UTIs.
Talk with a competent healthcare practitioner about getting a comprehensive nutrient test. Checking your vitamin D level is especially important since there is some evidence suggesting that vitamin D deficiency can contribute to incontinence. Once you are armed with the results, you can then determine the best plan of action to address any nutrient deficiencies or imbalances.
Since gluten can irritate the bladder, you may also want to talk with your doctor about eliminating it from your diet. In addition, make sure you drink enough water. I understand this may sound counterintuitive if you are trying to manage urinary incontinence, but it really isn’t. Not getting enough water can make your urine more concentrated, which can irritate your bladder.
Some foods can also aggravate incontinence since they can act as irritants to your urinary system or as diuretics which increase urine production. These include caffeine, carbonated beverages, alcohol, artificial sweeteners, spicy foods, dairy, chocolate, vinegar, soy sauce and citrus fruits.
Finally, review your current medications with your doctor to see if any of them may be causing or contributing to urinary incontinence.
Enjoy your healthy life!
Disclaimer: This article is not intended to provide medical advice. Please consult with your doctor or another competent healthcare practitioner to get specific medical advice for your situation.
The pH professional health care team includes recognized experts from a variety of health care and related disciplines, including physicians, attorneys, nutritionists, nurses, and certified fitness instructors. This team also includes the members of the pH Medical Advisory Board, which constantly monitors all pH programs, products, and services. To learn more about the pH Medical Advisory Board, click here.