It’s Not the Sexiest Topic, But Let’s Discuss Colonoscopies
6 years ago | Cancer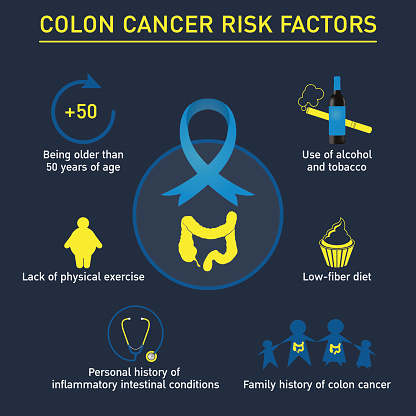
By Joy Stephenson-Laws, JD, Founder
I had my first colonoscopy when I turned 50 in 2010. So recently I decided I was due for a follow up since I am about to turn 60!
(It is recommended that persons like myself who have an average risk for colorectal cancer, should start getting colonoscopies at age 50. And then if all looks good, get one every 10 years, according to Harvard Health).
The results of my 2010 colonoscopy came back normal and healthy. So now I figured I would be proactive about my health and get another one. Afterall, it was time for my 10-year follow-up.
What was unusual about the second time around was that I was a lot more aware and educated about the procedure, so I asked a ton of questions. But before we get into all that, let's revisit some important issues.
- What exactly is a colonoscopy?
Basically, a colonoscopy is an outpatient procedure in which the inside of the large intestine (which consists of the colon and rectum and is about three to four feet long) is examined. This examination is done to look for abnormalities such as rectal and intestinal bleeding, polyps (abnormal tissue growths) and, most importantly, cancer.
- How does the doctor take a look inside my large intestine?
When you get a colonoscopy, the doctor uses an instrument called a colonoscope to examine the large intestine. The colonoscope is a long, flexible tubular device that is usually about half an inch in diameter, and it has the ability to transmit an image of the lining of the colon. I guess you can kind of think of it as an ultrasound of your colon. The colonoscope has a lens and light source that allows the doctor to review the images on a video monitor, which I got to see and ask questions about because I wasn’t completely knocked out!
- How does it feel?
Be prepared to get personal.
If you haven’t guessed by now, the colonoscope is inserted into the rectum.
“The scope bends, so the doctor can move it around the curves of your colon. You may be asked to change position occasionally to help the doctor move the scope. The scope also blows air into your colon, which expands the colon and helps the doctor see more clearly,” according to this source.
“You may feel mild cramping during the procedure. You can reduce the cramping by taking several slow, deep breaths during the procedure. When the doctor has finished, the colonoscope is slowly withdrawn while the lining of your bowel is carefully examined.”
Before you go running for the hills, hear me out.
The actual procedure usually takes about 30 minutes. In addition to this, you will be given intravenous medication that will make you feel relaxed and sedated. More importantly, it’s a procedure which is extremely necessary in order to be proactive about preventing colorectal cancer. And here’s why:
According to the American Cancer Society, excluding skin cancers, colorectal cancer (which is commonly called just colon cancer) is the third most common cancer diagnosed in both men and women in the United States. The American Cancer Society also predicts that in 2019 there will be 101,420 new cases of colon cancer and 44,180 new cases of rectal cancer.
In addition to this, the Centers for Disease Control and Prevention (CDC) reports that colorectal cancer is the second leading cancer killer.
And colonoscopies save lives.
Back in 2012, a study led by researchers at Memorial Sloan Kettering Cancer Center showed that "removing polyps by colonoscopy not only prevents colorectal cancer from developing, but also prevents deaths from the disease," according to the center's report discussing the study.
- Why should we care about polyps?
Polyps are abnormal tissue growths, but there is a bit more to them than that.
"The vast majority of polyps are NOT cancerous or even pre-cancerous. The polyps without the potential to turn into cancer include small hyperplastic polyps, inflammatory polyps, and hamartomatous polyps which are not part of an inherited polyp syndrome. The precancerous polyp which can turn into a cancer is called an adenoma," reports the American College of Gastroenterology.
"The two most common types of colorectal polyps are hyperplastic polyps and adenomas. Usually, the larger the size of the adenoma, the greater the chance that there may be cancer or pre-cancerous cells present in the polyp. Since it is hard to determine the exact nature of a polyp, polyps found during colonoscopy are removed and sent to the lab for a microscopic analysis."
So, the Sloan Kettering study involved 2,602 patients who had precancerous polyps (adenomas) removed during a colonoscopy. And the patients were evaluated for up to 23 years after they had their colonoscopies.
The study results revealed that the detection and removal of these polyps resulted in a 53 percent reduction in colorectal cancer mortality “compared to that of the deaths expected in the general population of comparable size, age, and gender. Furthermore, patients who had adenomatous polyps removed also had the same low death rate from colorectal cancer for up to 10 years after the procedure compared to a control group of people in whom no such polyps were detected.”
Furthermore, a more recent study involving 25,000 patients in the Veterans Affairs health system found that “colonoscopy was associated with a 61 percent reduction in colorectal cancer mortality," said one of the leads of the study, who was referenced in this report.
- So what were the results of my colonoscopy?
Of course I’m happy that I am proactive about my health, because my most recent colonoscopy revealed that I had a polyp. It was removed and sent to be biopsied. However, my doctor told me I don’t have much to be concerned about. And although colorectal cancer is the second-leading cause of cancer death, it is also one of the most preventable of all cancers.
So like I always say, prevention is better than cure.
To really put this all into perspective, if I hadn’t done my due diligence and got my recent colonoscopy, this could have been devastating. Colorectal cancer symptoms often don’t appear until after the cancer has grown or spread, according to the American Cancer Society.
Colonoscopies can save lives!
- How do you prepare for a colonoscopy?
In my opinion, preparing for a colonoscopy is worse than the actual procedure. The day before you get a colonoscopy, you have to take medications to induce diarrhea and clear the bowels. Clearing bowels is important so that the colonoscopy can identify early growths of colon cancer while they are treatable and before they spread. And of course, polyps (which can develop into cancer) can also be removed.
- Are there other screenings you can undergo for colorectal cancer?
There are several other types of colorectal screening and detection tests such as:
- Stool test
- Radiological imaging (virtual colonoscopy)
- Flexible sigmoidoscopy
“However, colonoscopy is the only test in which the entire colon can be visualized using a colonoscope and pre-cancerous polyps can be removed. Cancer risk is reduced 90 percent after colonoscopy and polyp removal, the American College of Gastroenterology estimates,” according to this source.
In addition to this, if you undergo a different type of screening and cancer cells are detected, you will need a follow-up colonoscopy anyway. A quality colonoscopy is the only screening that can both detect and prevent colorectal cancer.
So stop procrastinating and just get it over with! You only have to do it once every 10 years (in most cases) once you turn 50.
- How to make sure you are getting the best colonoscopy?
"It is now clear that not every colonoscopy is equal," says one doctor, in this report.
"Once you've decided it's time to get a screening colonoscopy, the next step is to make sure that you get a high quality one.”
Read here for three factors you may want to consider when looking for a specialist to do your colonoscopy.
- Are there risks with seniors and colonoscopies?
One study suggests that adults 75 and older may not need colonoscopies.
“Colon cancer tends to progress slowly, Sheffield [one of the doctors referenced] said, so early detection is less likely to benefit older adults. At the same time, colonoscopies come with the risk of complications, such as perforation of the intestine, bleeding or incontinence,” according to this report discussing the study.
Whatever your age, seek the advice of a competent healthcare professional regarding getting a colonoscopy.
- Should young people be thinking about colon cancer?
It may seem like you don’t even need to worry about colorectal cancer until you reach the age of 50, but this is certainly not the case. I previously discussed how one recent study led by the American Cancer Society suggested that those born in 1990 have double the risk of colon cancer and quadruple the risk of rectal cancer compared to people born around 1950.
This may be due to high rates of obesity in young people (being overweight is a risk factor for colorectal cancer).
And as with most cancers and disease, we can be proactive in preventing by following a nutrient-dense diet that is rich in plenty of fresh fruits, vegetables and whole foods.
For additional information on how you can be proactive about preventing colorectal cancer, click here.
Enjoy your healthy life!
The pH professional health care team includes recognized experts from a variety of health care and related disciplines, including physicians, attorneys, nutritionists, nurses and certified fitness instructors. This team also includes the members of the pH Medical Advisory Board, which constantly monitors all pH programs, products and services. To learn more about the pH Medical Advisory Board, click here.







