Your Blood Chemistry and Covid-19: What You Need to Know

By Joy Stephenson-Laws, JD, Founder
Healthcare providers and researchers continue to learn more about the SARS-CoV-2 virus (the virus that causes Covid-19) and how it impacts the body and its various systems. One key area of investigation has been why and how this novel coronavirus can trigger a level of blood clotting that can damage the lungs, heart and other organs.
Given how often doctors encounter this type of clotting in patients with severe Covid-19, along with rapidly-changing and at times conflicting media coverage of this aspect of Covid-19, it would be totally understandable if you have questions about blood clotting and what you can do to be proactive about blood health.
First off, let’s talk about what blood clotting is and why it’s important to your health. Also known as coagulation, it is the process by which your blood literally changes from a liquid to a gel-like consistency as a result of a cut or other damage to an artery or vein. Without the ability to form blood clots, which happens to people with hemophilia, you would bruise more easily and any cut or other damage to your circulatory system could result in you literally bleeding to death.
Blood clotting is really that important!
Most of the time, this process of clotting happens exactly the way it is supposed to: the body detects damage to an artery or vein, it triggers the clotting process to seal the wound and stop bleeding and the body goes on to heal.
At other times, however, more clotting happens than is required to repair any vascular damage, and the clots can then go on to cause such things as a heart attack, stroke, pulmonary embolism in your lungs or any number of other serious medical conditions. This is what doctors have been observing in patients with severe cases of Covid-19 – blood clots that are either not needed to stem any bleeding or an excessive amount of clotting taking place if it is necessary that begin to create risks to the patients’ health.
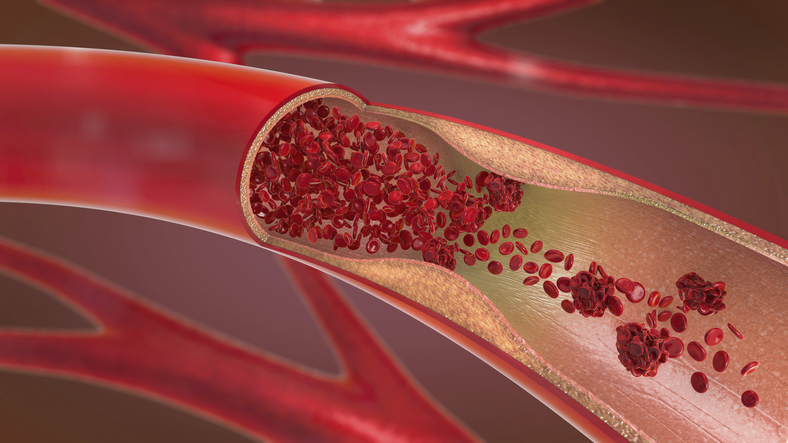
As you can imagine, being able to predict which patients may be at potentially greater or lesser risk for the type of clotting that Covid-19 can trigger could help provide them with potentially timelier and more effective treatment. To that end, researchers have recently hypothesized that the von Willebrand factor (VWF), a key component of blood clotting, may be associated with a more severe case of Covid-19. Their idea is that as the virus replicates, it causes microdamage to the walls of veins and arteries. This damage triggers the release of VWF into the blood to try to repair this damage and any “holes” it may have caused in the blood vessels. When this happens, the person has an increased risk of having that type of blood clot impact the brain, heart, lungs or other organs.
It is suggested that one reason why patients of the same age and health may react so differently to the new virus may be the level of VWF in their blood. If this turns out to be the case, it could help explain why some patients have no symptoms at all while others may become so ill that they require time in the Intensive Care Unit (ICU) with ventilator support.
Apparently, VWF’s main function is to create a framework or matrix for blood platelets to attach to during the clotting process. But the amount of VWF varies from person to person. While there are some individuals who have very low levels of VWF due to a hereditary disease known as von Willebrand disease (which is characterized by spontaneous bleeding), the levels can vary even among people who do not have the disease. For example, it is higher among African Americans when compared to Europeans; in men when compared to women; and in adults when compared to children. Coincidently, African Americans, men and adults have been shown to have a higher risk of developing more severe symptoms and complications from Covid-19.
Another area of blood chemistry that researchers are examining is blood type. Some recent studies suggest that individuals with Type O blood have lower levels of VWF while those with Type A tend to have higher amounts of VWF in their blood. Again, coincidently, some researchers are suggesting that persons with Type O blood may have a lower risk of contracting SARS-CoV-2 and developing more severe symptoms while those with Type A may have a greater risk.
How to promote blood and cardiovascular health.While you cannot change your blood type or readily decrease the amount of VWF in your blood, there are things that you can do to promote better cardiovascular health and possibly reduce the impact the virus could have on this system.
One of the most important things you can do is take steps to reduce any chronic inflammation you may currently have since this condition has been linked to coagulation and clotting. This type of inflammation, as compared to the perfectly normal and healthy immune response of acute inflammation in response to an injury, can last several months or even years. It is essentially believed to be the root cause of many diseases Americans face. For example, in certain cases, chronic inflammation has been linked to arteriosclerosis (narrowing of the arteries).
One of the primary causes of chronic inflammation is obesity, so it’s important to maintain a healthy weight. Other causes are smoking, chronic stress and excessive alcohol consumption.
Making healthy lifestyle choices may also reduce chronic inflammation as well as promote cardiovascular health. In addition to not smoking and maintaining a healthy weight, you should also aim to get at least 150 minutes a week of moderate exercise (such as walking or biking), getting enough sleep (between 7 and 8 hours a night for most people) and staying hydrated.
Of course, making sure your cardiovascular system is getting the nutrients it needs – and in the right amounts – is equally important. These nutrients include iron, copper, zinc, fiber, omega-3 fatty acids and magnesium. You can get all of these by eating a primarily plant-based diet since fresh fruits and vegetables are nutrient dense. Some great foods and seasonings for your cardiovascular system include cayenne pepper, onions, garlic, fatty fish, beets, leafy greens such as spinach, turmeric, walnuts and, one of my favorites, citrus fruits. Also consider adding tomatoes and berries to the mix.
When it comes to reducing chronic inflammation, the first thing you should do is test your blood for inflammation markers so that you and your doctor, or other competent healthcare professional, can better identify the cause of the inflammation and what you can do to reduce or eliminate it altogether. Diet also plays a role in reducing inflammation and the good news is that many of the same foods that are good for your cardiovascular system also have anti-inflammatory properties. In addition to those mentioned above, you can have avocados, green tea, extra virgin olive oil, grapes, mushrooms and dark chocolate and cocoa. If you like cherries, you’re in luck since they are rich in antioxidants that fight inflammation.
There are also foods that you should try and avoid, such as junk foods (of course), refined carbohydrates such as white bread and pasta, fried foods, sugary beverages, processed meats such as bacon and salami and trans fats such as margarine.
Enjoy your healthy life!
Disclaimer: This article is not intended to provide medical advice. Please consult with your doctor or another competent healthcare practitioner to get specific medical advice for your situation.
The pH professional health care team includes recognized experts from a variety of health care and related disciplines, including physicians, attorneys, nutritionists, nurses and certified fitness instructors. This team also includes the members of the pH Medical Advisory Board, which constantly monitors all pH programs, products and services. To learn more about the pH Medical Advisory Board, click here.







